Credentialing vs. Enrollment: Understanding the Difference and Why It Matters
Introduction
Confused between “credentialing” and “provider enrollment”? You’re not alone. These terms are often used interchangeably—but they involve distinct processes, each critical for timely reimbursement and compliance. At MediCloud Billing Solution LLC, we help providers and medical groups navigate both with clarity and confidence.
Defining the Two Terms
| Credentialing | Enrollment |
| Verifies qualifications and background | Registers provider with insurers |
| Includes license checks, work history, education | Includes credentialing + payer contract setup |
| Required for payer participation | Required for claim reimbursement |
Credentialing in Detail
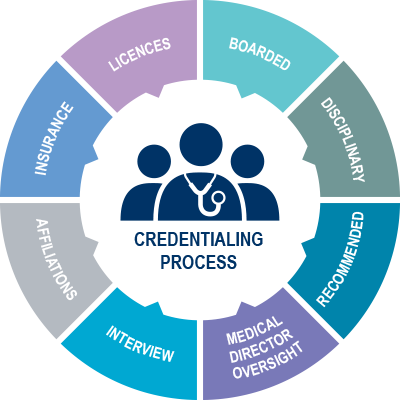
Credentialing ensures that a provider is qualified and authorized to deliver care. It involves:
- Education verification
- License and DEA checks
- Reference checks
- Malpractice claims review
- CAQH attestation
Credentialing must be performed:
- Upon hiring a new provider
- Every 2–3 years (recredentialing)
- When switching organizations
Enrollment in Detail
Enrollment builds on credentialing and adds:
- NPI matching
- Tax ID and entity validation
- Payer contracts and rate agreements
- Effective date confirmation
Enrollment timelines:
- Medicare: 60–90 days via PECOS
- Medicaid: 30–120 days, varies by state
- Commercial: 45–90 days average
Why It Matters
Failing to complete either process correctly can result in:
- Denied claims
- Delayed revenue
- Compliance violations
- Audit risks
Our Credentialing & Enrollment Services Include:
✅ CAQH creation and updates
✅ PECOS and Medicaid submission
✅ Commercial payer contracting
✅ DEA, board, and license verification
✅ Follow-up and appeals support
Conclusion
Knowing the difference between credentialing and enrollment can save your practice time, money, and frustration. At MediCloud, we ensure every provider meets the highest standards—and gets enrolled without delays.
Top 10 Article Categories
- Medical Coding Updates & Guidelines
- Revenue Cycle Management Best Practices
- Medical Billing Compliance & Regulations
- Denial Management and Appeals
- Healthcare Payer Policies & Reimbursement Trends
- Practice Management & Billing Software Tips
- Provider Enrollment & Credentialing Essentials
- Specialty-Specific Billing Challenges
- Insurance Verification & Patient Eligibility
- Telemedicine Billing and Coding
Blogs
Understand the billing and coding process through our comprehensive articles that offer insightful tips and tricks.
Articles
Understand the billing and coding process through our comprehensive articles that offer insightful tips and tricks.


