Navigating Pharmacy Prior Authorizations and Insurance Verification
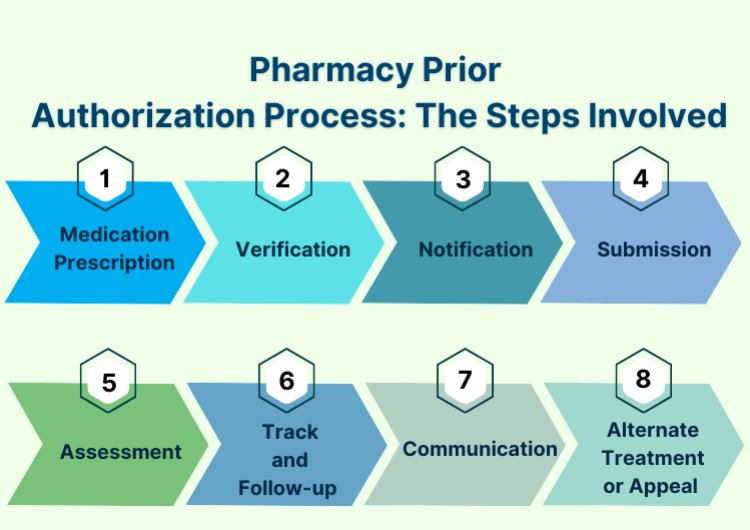
Prior authorization and insurance verification are essential in pharmacy billing. Missing approvals or incorrect insurance details can cause claim denials and delays in patient medication delivery.
Our experts at MediCloud Billing Solution LLC manage these processes efficiently to minimize disruptions and improve your reimbursement rates.
Benefits of Expert Prior Authorization Management:
- Fewer rejected claims
- Faster patient access to medications
- Streamlined workflow for pharmacy staff
Partner with us to ensure smooth prior authorization handling.
BLOGS
Blogs
Understand the billing and coding process through our comprehensive articles that offer insightful tips and tricks.
Articles
Understand the billing and coding process through our comprehensive articles that offer insightful tips and tricks.


